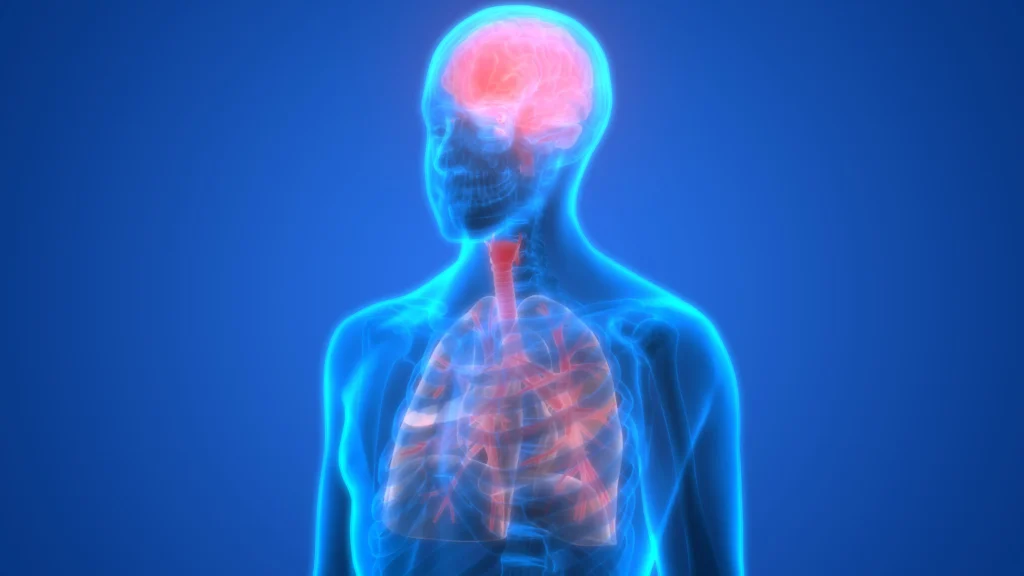
The concept of the brain – lung axis refers to a bidirectional communication pathway between the brain and the lungs. Breathing, for example, does more than just deliver oxygen to your lungs—it also sends neural signals to your brain, and vice versa.
In fact, research has shown that breathing patterns influence brain health: slow, controlled breathing promotes mental relaxation and calm, whereas rapid breathing can trigger feelings of anxiety. Moreover, the vagus nerve reinforces this axis by swiftly conveying information from the lungs to the brain and by regulating inflammatory interactions in both organs via neurotransmitters such as acetylcholine.
——- Ad ——-
——- Ad ——-
Communication Pathways Between Lung and Brain
The lungs and brain communicate through several channels:
● Neural Pathway
Nerves are the most direct routes between lungs and brain. Here, the vagus nerve carries sensory signals from the lungs up to brain centers that then adjust respiratory and other functions. Other sensory nerves in the lungs detect changes (e.g. stretch, irritation) and instantly activate specific neural circuits in the brain, producing physical and psychological symptoms. Studies further indicate that stimulating these neural routes can reduce inflammation in both the respiratory and central nervous systems.
● Immune Pathway
The immune system forms another communication conduit. When lung tissue is infected or inflamed, immune cells release protein messengers called cytokines into the bloodstream. These cytokines can cross the blood–brain barrier (BBB) and help coordinate recovery processes in the brain.
However, excessive cytokine levels may provoke neuroinflammation and impair cognitive function. For example, after severe pulmonary infections, elevated inflammatory cytokines in the brain are thought to drive cognitive decline. Thus, lung-driven immune responses alert the brain—and vice versa—opening the door to integrated therapies targeting both systems simultaneously.
● Microbiological Pathway
Much like the gut, healthy lungs harbor a diverse microbiome whose constituents can also influence the brain. Researchers have found that lung microbes may contribute to neuroimmune conditions such as multiple sclerosis (MS). Certain bacterial components (e.g. lipopolysaccharide, LPS) can breach the blood–brain barrier and travel via the bloodstream to the brain, potentially initiating or worsening demyelinating processes. In this way, the lung microbiota form an indirect or direct line of communication with the central nervous system.
——- Ad ——–
——- Ad ——–
Diseases Linked to the Brain–Lung Axis
Several disorders are now associated with dysregulation of the brain–lung axis:
1. Asthma
Asthma often coexists with neurological symptoms—such as poor concentration, anxiety, and sleep disturbances—suggesting that recurrent pulmonary inflammation sends signals to brain regions governing alertness and mood. Conversely, stress and anxiety originating in the brain can provoke bronchoconstriction and trigger asthma attacks.
2. Acute Pneumonia
Acute lung infections caused by bacteria, fungi, or viruses can allow microbial agents or their toxins to cross into the brain, leading to neurocognitive symptoms such as confusion or “brain fog.”
3. Depression
Impaired lung function has been linked to higher rates of depression. In a large cohort study of over 280,000 individuals, reduced pulmonary capacity correlated with increased depression risk—likely because diminished oxygen delivery impairs brain metabolism and mood regulation, Additionally, the physical limitations of poor respiratory health can hinder social engagement and communication, which are vital for mental well-being.
4. Traumatic Brain Injury (TBI)
Severe head injuries can precipitate acute lung complications—such as neurogenic pulmonary edema and ventilator‑associated pneumonia—due to excessive neural signaling that disrupts normal pulmonary function.
5. Stroke
Stroke patients face up to a 10% risk of developing pneumonia post‑event; Post-stroke pneumonia is a major cause of death, accounting for roughly two-thirds of all fatalities.
Conclusion
Understanding the brain–lung axis offers valuable clinical insights for treating both neurological and respiratory conditions. It paves the way for novel strategies—such as modulating immune responses or reshaping the pulmonary microbiome—to protect or restore the function of both organs. In sum, a deeper understanding of the intimate link between the lungs and brain holds great promise for improving the prevention and management of diseases affecting either system.
○ Share the article:
References
(1) Huang, S., Zhou, Y., Ji, H. et al. Decoding mechanisms and protein markers in lung-brain axis. Respir Res 26, 190 (2025).
(2) Wang, Y., Mou, Y. K., Wang, H. R., Song, X. Y., Wei, S. Z., Ren, C., & Song, X. C. (2023). Brain response in asthma: the role of “lung-brain” axis mediated by neuroimmune crosstalk. Frontiers in immunology, 14, 1240248.
(3) Chen, J., Li, T., Ye, C., Zhong, J., Huang, J. D., Ke, Y., & Sun, H. (2023). The Lung Microbiome: A New Frontier for Lung and Brain Disease. International journal of molecular sciences, 24(3), 2170.
(4) Ma, Q., Yao, C., Wu, Y., Wang, H., Fan, Q., Yang, Q., Xu, J., Dai, H., Zhang, Y., Xu, F., Lu, T., Dowling, J. K., & Wang, C. (2023). Neurological disorders after severe pneumonia are associated with translocation of endogenous bacteria from the lung to the brain. Science advances, 9(42), eadi0699.